Research Shows Targeted Radiotherapy Benefits Elderly Pancreatic Cancer Patients
 It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
The good news is that research shows that stereotactic body radiotherapy (SBRT) — a form of radiation therapy that uses a highly targeted beam of radiation to kill cancer cells while leaving the healthy tissue around the tumor unharmed — is highly effective for treating the symptoms of pancreatic cancer even in patients not healthy enough to undergo more invasive traditional treatments. A study performed at Detroit’s Henry Ford Hospital found that SBRT was able to significantly slow the progression of pancreatic cancer.
SBRT Improves Pancreatic Cancer Prognosis
Most people diagnosed with pancreatic cancer are over age 65, and for many, the prognosis is unpleasant. Without some form of treatment, most pancreatic cancer patients will not live more than four to six months.
 Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
The physicians found that SBRT was able to slow the spread of pancreatic cancer for five to six months. One-third of the patients lived more than a year thanks to SBRT. The patients reported minimal side effects.
In a second study published in 2013, physicians at the same hospital looked at the benefits of SBRT for 20 pancreatic cancer patients not considered able to tolerate either surgery or chemo-radiation therapy. These patients received SBRT treatments for an average of two weeks. Sixty-one percent of these patients survived for at least six months after treatment. These patients, too, experienced minimal side effects and were able to maintain a decent quality of life throughout treatment, the researchers report.
Benefits of Targeted Radiation Therapy
The Henry Ford Hospital physicians involved in these two studies believe that SBRT treatment, like the treatment delivered at our Los Angeles cancer center, is more effective than traditional radiation therapy. For one thing, SBRT allows physicians to administer a higher dose of radiation that kills cancer cells more aggressively, but because the radiation is targeted at the site of the tumor, there’s little to no damage to healthy tissue. Because the dose of radiation is higher, patients can spend less time in therapy and more time enjoying their lives.
SBRT may be the only option for pancreatic cancer treatment for a fraction of patients who are not good candidates for surgery, chemotherapy, or traditional radiation therapy. For these patients, SBRT can mean an improved prognosis and better quality of life throughout the course of treatment, since it can be completed in just two weeks and causes minimal side effects.
More
Study Links Vasectomy to Prostate Cancer
 A new study from the Harvard School of Public Health (HSPH) has found that men who have vasectomies are at an increased risk of developing prostate cancer. The researchers found no significant increase in the risk of low-grade prostate cancer among men with vasectomies, but instead found that those who had undergone the sterilization procedure had a higher risk of advanced and lethal prostate cancer. Overall, men who had vasectomies had about a 10 percent higher risk of prostate cancer than those who had not.
A new study from the Harvard School of Public Health (HSPH) has found that men who have vasectomies are at an increased risk of developing prostate cancer. The researchers found no significant increase in the risk of low-grade prostate cancer among men with vasectomies, but instead found that those who had undergone the sterilization procedure had a higher risk of advanced and lethal prostate cancer. Overall, men who had vasectomies had about a 10 percent higher risk of prostate cancer than those who had not.
Largest Ever Study into Vasectomy/Prostate Cancer Link
The HSPH study, which appeared online in the Journal of Clinical Oncology on July 7, 2012, is the most comprehensive such study to look at the link between vasectomy and prostate cancer risk. It was a follow-up to HSPH’s 1993 study on vasectomy and prostate cancer risk. The researchers followed 49,405 men for 24 years, from 1986 to 2010. Twenty-five percent of the men in the study had had a vasectomy.
Over the course of the study period, 6,023 men were diagnosed with prostate cancer. 811 of those died of prostate cancer. The researchers found that a previous vasectomy was associated with a 20 percent higher risk of advanced prostate cancer and a 19 percent higher risk of lethal prostate cancer. Among men who received regular PSA screenings, the relative increase in lethal prostate cancer risk was 56 percent.
The researchers found that the younger a man was at the time of his vasectomy, the greater his risk for advanced or lethal prostate cancer. Men who had had their vasectomies before 38 years of age were found to be at the highest risk.
Researchers Rule out Bias
Previous studies into the possibility of a link between vasectomy and prostate cancer may have been biased. For one thing, men who receive vasectomies tend to receive better medical care and more regular PSA screening, meaning that they’d be more likely than men who did not receive vasectomies to be diagnosed with prostate cancer.
Nor could previous studies rule out the possibility that sexually transmitted infections or other potential risk factors may have contributed to higher rates of prostate cancer among study participants. For this study, however, researchers had access to enough information about the study participants to rule out these potential biases.
Overall Increase in Risk Is Small
 If you’re one of the 15 percent of American men who have had a vasectomy, don’t panic yet. The overall increase in prostate cancer risk for men who have had vasectomies is small — just 10 percent.
If you’re one of the 15 percent of American men who have had a vasectomy, don’t panic yet. The overall increase in prostate cancer risk for men who have had vasectomies is small — just 10 percent.
Since previous research has failed to find a clear-cut link between vasectomy and prostate cancer, many experts advise taking these findings with a grain of salt. Prostate cancer treatments are steadily improving, and most men diagnosed with the disease don’t die from it.
Dr. Louis Kavoussi, chairman of urology at North Shore-LIJ Health System in New Hyde Park, N.Y., told CBS News, “I would be cautious about applying these findings to clinical practice right now. This is not like cigarette smoking causing a large number of people to develop lung cancer. This is a small increase in the risk of prostate cancer.”
New data from a HSPH study found a link between vasectomy and prostate cancer. Men who have had vasectomies are 10 percent more likely to develop prostate cancer. If you have had a vasectomy, don’t let it keep you up at night — experts say the relative increased risk is small.
More
The following is a White Paper on CyberKnife’s ability to treat Lung Metastases.
White Paper Cyberknife for Lung Metastases
More
The following study shows the importance of real-time image guidance and robotic motion-compensation techniques used in CyberKnife.
Purpose
To report the characteristics of prostate motion as tracked by the stereoscopic X-ray images of the implanted fiducials during hypofractionated radiotherapy with CyberKnife.
Methods and Materials
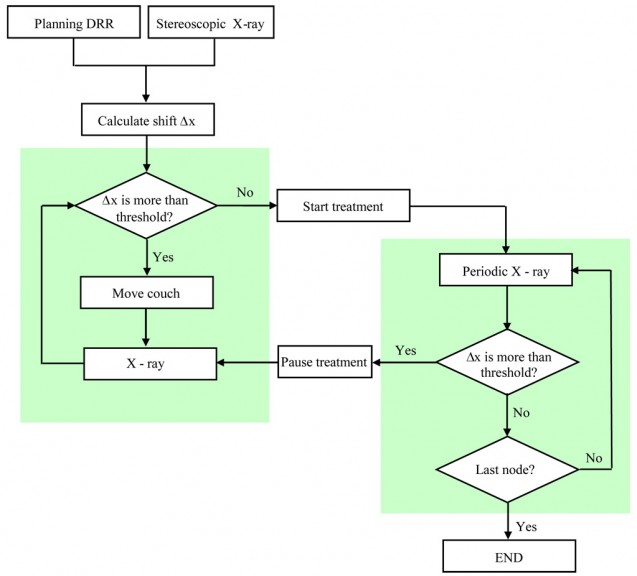
Twenty one patients with prostate cancer who were treated with CyberKnife between January 2005 and September 2007 were selected for this retrospective study. The CyberKnife uses a stereoscopic X-ray system to obtain the position of the prostate target through the monitoring of implanted gold fiducial markers. If there is a significant deviation, the treatment is paused while the patient is repositioned by moving the couch. The deviations calculated from X-ray images acquired within the time interval between two consecutive couch motions constitute a data set.
Results
A total of 427 data sets and 4439 time stamps of X-ray images were analyzed. The mean duration for each data set is 697 s. At 30 s, a motion larger than 2 mm exists in about 5% of data sets. The percentage is increased to 8%, 11%, and 14% at 60 s, 90 s, and 120 s, respectively. A similar trend exists for other values of prostate motion.
Conclusions
With proper monitoring and intervention during treatment, the prostate shifts observed among the patients can be kept within the tracking range of the CyberKnife. On average a sampling rate of ~40 s between consecutive X-rays is acceptable to ensure sub-millimeter tracking. However, there is significant movement variation among patients and higher sampling rate may be necessary in some patients.
More
Here’s another case study we would like to share:
Amy (name has been changed to protect patient’s privacy) is a 48-year-old female diagnosed with bone sarcoma and underwent below-knee amputation of right leg 3 years ago. Unfortunately, she developed multiple metastases in both lungs a year later. She decided to undergo two aggressive surgeries and more than 10 lesions were removed from each lung. She also received chemotherapy following the surgeries.
Earlier this year, Amy was found to have 2 recurrent lung metastases which are located in areas of the lung that are difficult to resect. Her lung function has greatly decreased in the past 2 years due to the surgeries she underwent. As a result, she was skeptical and went in search for other options. One of her friends, who was recently treated at our center, advised her to contact us. After consulting with Dr. Albert Mak and her medical oncologist, it was determined that she was a good candidate for the CyberKnife radiosurgery treatment. Amy was still very nervous about this radiosurgical procedure we recommended because she did not want to undergo further surgery. Although the name CyberKnife suggests scalpels, operating rooms and recovery time, it actually involves no incisions, no anesthesia, no pain and no hospital stay. The CyberKnife is indeed a knifeless outpatient procedure. After careful consideration and weighing her options, Amy decided rather quickly to have the CyberKnife treatment.
Due to the size and location of her lesions, we recommended two separate courses of treatment. During the first course of treatment, we focused on treating the larger tumor. The first course was only 3 days, and each treatment took about 45 minutes. The CyberKnife treatment is a painless and non-invasive procedure which was a big thumbs up for Amy. Unlikely other radiosurgical devices, no immobilization device is needed for CyberKnife. The robot continuously tracked Amy’s lung lesions and adjusted for movement. As a result of this unique tracking capability only available with the CyberKnife system, Amy did not have to hold her breath during treatment and was able to breathe normally and relax comfortably.
Amy tolerated the short course of 3-day treatment very well. She also underwent chemotherapy during the CyberKnife treatment. It has been a month since her first treatment, and we are happy to report that the follow-up CT scan shows that the tumor was reduced by half. She feels very optimistic and hopeful for the future, and will start her second course of treatment next week.
If you would like more information on CyberKnife treatment for lung cancer and pulmonary metastases, please do not hesitate to contact our center at 626-768-1021.
More
 It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes. Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.