Research Shows Targeted Radiotherapy Benefits Elderly Pancreatic Cancer Patients
 It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
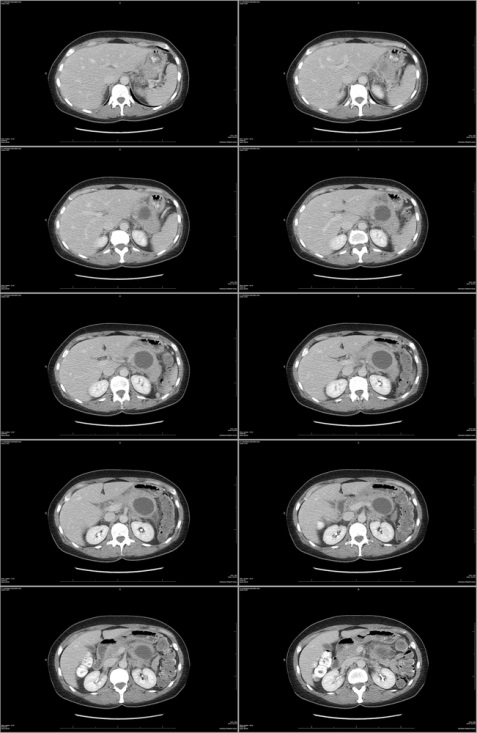
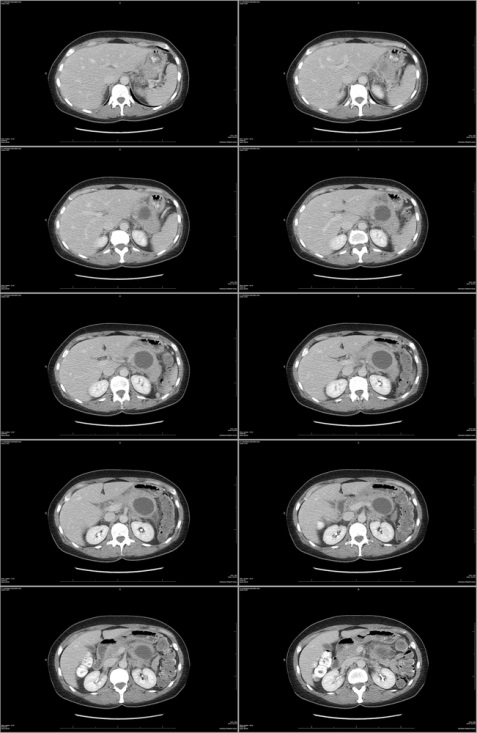
The good news is that research shows that stereotactic body radiotherapy (SBRT) — a form of radiation therapy that uses a highly targeted beam of radiation to kill cancer cells while leaving the healthy tissue around the tumor unharmed — is highly effective for treating the symptoms of pancreatic cancer even in patients not healthy enough to undergo more invasive traditional treatments. A study performed at Detroit’s Henry Ford Hospital found that SBRT was able to significantly slow the progression of pancreatic cancer.
SBRT Improves Pancreatic Cancer Prognosis
Most people diagnosed with pancreatic cancer are over age 65, and for many, the prognosis is unpleasant. Without some form of treatment, most pancreatic cancer patients will not live more than four to six months.
 Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
The physicians found that SBRT was able to slow the spread of pancreatic cancer for five to six months. One-third of the patients lived more than a year thanks to SBRT. The patients reported minimal side effects.
In a second study published in 2013, physicians at the same hospital looked at the benefits of SBRT for 20 pancreatic cancer patients not considered able to tolerate either surgery or chemo-radiation therapy. These patients received SBRT treatments for an average of two weeks. Sixty-one percent of these patients survived for at least six months after treatment. These patients, too, experienced minimal side effects and were able to maintain a decent quality of life throughout treatment, the researchers report.
Benefits of Targeted Radiation Therapy
The Henry Ford Hospital physicians involved in these two studies believe that SBRT treatment, like the treatment delivered at our Los Angeles cancer center, is more effective than traditional radiation therapy. For one thing, SBRT allows physicians to administer a higher dose of radiation that kills cancer cells more aggressively, but because the radiation is targeted at the site of the tumor, there’s little to no damage to healthy tissue. Because the dose of radiation is higher, patients can spend less time in therapy and more time enjoying their lives.
SBRT may be the only option for pancreatic cancer treatment for a fraction of patients who are not good candidates for surgery, chemotherapy, or traditional radiation therapy. For these patients, SBRT can mean an improved prognosis and better quality of life throughout the course of treatment, since it can be completed in just two weeks and causes minimal side effects.
More
5 Pancreatic Cancer Myths, Busted
 Pancreatic cancer has a bad reputation. It’s known for being one of the most difficult cancers to treat, in part because its early symptoms can be so difficult to pinpoint. Symptoms like jaundice, loss of appetite, abdominal pain, weight loss and general weakness can be indicative of a range of health problems — they aren’t necessarily pancreatic cancer. Plus, there’s no basic diagnostic test that can help physicians screen for pancreatic cancer. Myths about this scary form of cancer abound, but it’s important that you have the facts about pancreatic cancer if you want to defeat it.
Pancreatic cancer has a bad reputation. It’s known for being one of the most difficult cancers to treat, in part because its early symptoms can be so difficult to pinpoint. Symptoms like jaundice, loss of appetite, abdominal pain, weight loss and general weakness can be indicative of a range of health problems — they aren’t necessarily pancreatic cancer. Plus, there’s no basic diagnostic test that can help physicians screen for pancreatic cancer. Myths about this scary form of cancer abound, but it’s important that you have the facts about pancreatic cancer if you want to defeat it.
Myth 1: Pancreatic Cancer Is Always Deadly
Let’s get this damaging myth out of the way first. Pancreatic cancer is not always deadly — far from it. Like other forms of cancer, early detection is the key to successful treatment. Five-year survival rates are highest among those who are diagnosed early, and advances in pancreatic cancer treatment have made the disease much more survivable than it has been in the past. If you’re worried about developing pancreatic cancer, don’t be — it’s a relatively rare form of cancer, occurring in about 30,000 people a year. Just five to ten percent of cases are hereditary.
Myth 2: Pancreatic Cancer Screening Tests Are Available and Common
Unfortunately, pancreatic cancer screening tests are not commonly done. In fact, researchers have not yet developed an easy and accurate way to screen for pancreatic cancer. Unlike prostate or breast cancers, for example, there’s no blood test or specific imaging procedure that can reliably detect this cancer. CT scans can detect prostate tumors, but only a biopsy can determine if those tumors are cancerous.
Myth 3: There Is Only One Kind of Prostate Cancer
There are actually two kinds of pancreatic cancer. The vast majority — 95 percent — of pancreatic cancers are of a type known as adenocarcinoma. These tumors arise in the ductal cells that line the pancreatic ducts. The other, rarer form of pancreatic cancer occurs in the islets of Langerhans, the cells of the pancreas itself, where insulin is made. Cancer in these cells is known as islet-cell pancreatic cancer.
Myth 4: You Should Avoid Physical Contact with Others During Radiation Therapy
 This myth arose out of an understandable concern that radiation treatment could actually make a patient radioactive, placing his or her friends and loved ones at risk. However, the radiation used to treat pancreatic cancer doesn’t hang around in the body.
This myth arose out of an understandable concern that radiation treatment could actually make a patient radioactive, placing his or her friends and loved ones at risk. However, the radiation used to treat pancreatic cancer doesn’t hang around in the body.
Once you have finished a treatment session, you can feel free to go home and hug your loved ones at will. They are not at risk of being exposed to radiation because you are going through treatment. Physical contact with loved ones can be beneficial for all of you.
Myth 5: Surgery Makes Pancreatic Cancer More Likely to Spread
Lots of people know somebody who received surgery for pancreatic cancer, or another type of cancer, only to find that their cancer metastasized after surgery. However, it’s a myth that surgery for pancreatic cancer can cause it to spread by exposing the cancer to the air or lowering immunity. Surgery can’t cause cancer to spread, but it can prevent it from spreading.
The more you know about pancreatic cancer, the better your chances of recovering from it. With early detection and the right treatment plan, you can put pancreatic cancer behind you — where it belongs.
More
Study Links Vasectomy to Prostate Cancer
 A new study from the Harvard School of Public Health (HSPH) has found that men who have vasectomies are at an increased risk of developing prostate cancer. The researchers found no significant increase in the risk of low-grade prostate cancer among men with vasectomies, but instead found that those who had undergone the sterilization procedure had a higher risk of advanced and lethal prostate cancer. Overall, men who had vasectomies had about a 10 percent higher risk of prostate cancer than those who had not.
A new study from the Harvard School of Public Health (HSPH) has found that men who have vasectomies are at an increased risk of developing prostate cancer. The researchers found no significant increase in the risk of low-grade prostate cancer among men with vasectomies, but instead found that those who had undergone the sterilization procedure had a higher risk of advanced and lethal prostate cancer. Overall, men who had vasectomies had about a 10 percent higher risk of prostate cancer than those who had not.
Largest Ever Study into Vasectomy/Prostate Cancer Link
The HSPH study, which appeared online in the Journal of Clinical Oncology on July 7, 2012, is the most comprehensive such study to look at the link between vasectomy and prostate cancer risk. It was a follow-up to HSPH’s 1993 study on vasectomy and prostate cancer risk. The researchers followed 49,405 men for 24 years, from 1986 to 2010. Twenty-five percent of the men in the study had had a vasectomy.
Over the course of the study period, 6,023 men were diagnosed with prostate cancer. 811 of those died of prostate cancer. The researchers found that a previous vasectomy was associated with a 20 percent higher risk of advanced prostate cancer and a 19 percent higher risk of lethal prostate cancer. Among men who received regular PSA screenings, the relative increase in lethal prostate cancer risk was 56 percent.
The researchers found that the younger a man was at the time of his vasectomy, the greater his risk for advanced or lethal prostate cancer. Men who had had their vasectomies before 38 years of age were found to be at the highest risk.
Researchers Rule out Bias
Previous studies into the possibility of a link between vasectomy and prostate cancer may have been biased. For one thing, men who receive vasectomies tend to receive better medical care and more regular PSA screening, meaning that they’d be more likely than men who did not receive vasectomies to be diagnosed with prostate cancer.
Nor could previous studies rule out the possibility that sexually transmitted infections or other potential risk factors may have contributed to higher rates of prostate cancer among study participants. For this study, however, researchers had access to enough information about the study participants to rule out these potential biases.
Overall Increase in Risk Is Small
 If you’re one of the 15 percent of American men who have had a vasectomy, don’t panic yet. The overall increase in prostate cancer risk for men who have had vasectomies is small — just 10 percent.
If you’re one of the 15 percent of American men who have had a vasectomy, don’t panic yet. The overall increase in prostate cancer risk for men who have had vasectomies is small — just 10 percent.
Since previous research has failed to find a clear-cut link between vasectomy and prostate cancer, many experts advise taking these findings with a grain of salt. Prostate cancer treatments are steadily improving, and most men diagnosed with the disease don’t die from it.
Dr. Louis Kavoussi, chairman of urology at North Shore-LIJ Health System in New Hyde Park, N.Y., told CBS News, “I would be cautious about applying these findings to clinical practice right now. This is not like cigarette smoking causing a large number of people to develop lung cancer. This is a small increase in the risk of prostate cancer.”
New data from a HSPH study found a link between vasectomy and prostate cancer. Men who have had vasectomies are 10 percent more likely to develop prostate cancer. If you have had a vasectomy, don’t let it keep you up at night — experts say the relative increased risk is small.
More
What to Do When Cancer Treatment Causes Eating Problems
 Cancer treatment in general can make it hard to maintain adequate nutrition, but patients undergoing treatment for head and neck cancer in particular face a unique set of challenges. Targeted treatments seek to minimize side effects that can cause dry mouth, soreness of the mouth and throat, difficulty swallowing and mouth ulcers. But in spite of the best efforts of your treatment team, you may still experience some of these side effects.
Cancer treatment in general can make it hard to maintain adequate nutrition, but patients undergoing treatment for head and neck cancer in particular face a unique set of challenges. Targeted treatments seek to minimize side effects that can cause dry mouth, soreness of the mouth and throat, difficulty swallowing and mouth ulcers. But in spite of the best efforts of your treatment team, you may still experience some of these side effects.
When head and neck cancer treatment makes it hard to eat, you may need to change your eating habits accordingly. Soft foods and thick liquids are often easier to swallow when you’re suffering from soreness of the mouth and throat, and can even be soothing to irritated areas. At the same time, there are some foods you should avoid during head and neck cancer treatment, because they can irritate sensitive tissues. In order for head and neck cancer treatment to be a success, it’s important that you maintain proper nutrition and eat enough calories to keep up your strength.
Remember the Basics of Cancer Treatment Nutrition
When you’re having trouble chewing or swallowing your food due to the side effects of head and neck cancer treatment, the principles of good nutrition remain the same as if you were having any other kind of cancer treatment. You may need to switch to eating six to eight small meals each day instead of three big ones. You should also focus on eating calorie-dense, nutritious foods. You may not be able to eat as much as you could before you started treatment, so you need to make every mouthful count in terms of calories. Keep your diet balanced, too, by eating a variety of foods.
Make Foods Easier to Swallow
Thick liquids, like milkshakes and yogurt, can be easier to swallow than thin liquids when swallowing is difficult. You can add thickening agents, like gelatin or cornstarch, to thin soups, or use a slurry (mix of water and flour) to soften cakes and breads enough to swallow them comfortably. Use a blender or food processor to puree your meals.
Avoid Acidic, Spicy, Salty or Tart Foods
If you have soreness or ulcers in your mouth or throat, certain foods can aggravate that condition. These foods can include:
- Tart fruits and citrus fruits
- Pickled foods
- Foods, dressings and sauces containing vinegar
- Tomato-based sauces and foods
- Foods with a rough texture, like granola, toast or raw vegetables and fruits
- Spicy or peppery foods, like cloves, horseradish, chili pepper, nutmeg and hot sauces
 Use mild spices like rosemary, oregano, mint, basil and thyme to add flavor to your meals. Add calories to your diet using lean meats, peanut butter, dairy products, nuts and seeds, or liquid food supplements. If you have sores or ulcers in your mouth or throat, soft, bland foods are the way to go. Drink liquids through a straw to keep them from irritating sore areas. If you’re not sure what to eat, there are plenty of recipes designed for people going through head and neck cancer treatment available online.
Use mild spices like rosemary, oregano, mint, basil and thyme to add flavor to your meals. Add calories to your diet using lean meats, peanut butter, dairy products, nuts and seeds, or liquid food supplements. If you have sores or ulcers in your mouth or throat, soft, bland foods are the way to go. Drink liquids through a straw to keep them from irritating sore areas. If you’re not sure what to eat, there are plenty of recipes designed for people going through head and neck cancer treatment available online.
The most important thing to remember when you’re going through treatment for head and neck cancer is that you need to keep up your strength and minimize weight loss. Add calories to your diet whenever you can, to get the most out of your treatments.
More
Your Basic Guidebook to Prostate Cancer
 Prostate cancer is a disease that can only affect men. Unlike even breast cancer which though associated with women but can grow in both sexes, the prostate gland is as common a natural occurrence in the female body as ovaries are in men. The prostate is part of the male reproductive system and is responsible for the production of much of the volume of the seminal fluid. Cancer of the prostate gland is more commonly diagnosed than breast cancer, and it is gaining as much popularity as the pink-ribboned disease. Prostate cancer is often relatively slow growing and often shows no symptoms. In later stages, however, it can be responsible for diminished reproductive function, problems urinating, blood in the urine and pain in the back or pelvis when urinating.
Prostate cancer is a disease that can only affect men. Unlike even breast cancer which though associated with women but can grow in both sexes, the prostate gland is as common a natural occurrence in the female body as ovaries are in men. The prostate is part of the male reproductive system and is responsible for the production of much of the volume of the seminal fluid. Cancer of the prostate gland is more commonly diagnosed than breast cancer, and it is gaining as much popularity as the pink-ribboned disease. Prostate cancer is often relatively slow growing and often shows no symptoms. In later stages, however, it can be responsible for diminished reproductive function, problems urinating, blood in the urine and pain in the back or pelvis when urinating.
Risk Factors
The direct causes of prostate cancer are not entirely known but there are a few correlations to increased risk. Prostate cancer is significantly more prevalent in developed nations; however, this is largely due to the availability of medical testing increasing the rate of diagnosis. Also, race, diet, family history and obesity all can play a factor. There is a small increased risk of prostate cancer with lack of exercise.
High rates of red meat and dairy consumption increase the risk for prostate cancer. It’s possible this is due to a decrease in the rates of vegetable consumption that has a direct correlation with high red meat diets. Also, men who have a first-degree relative (father or brother) with prostate cancer are twice as likely to be diagnosed in their lifetime; this soars to five times as likely with two or more first-degree relatives diagnosed.
Survival Rates
Luckily, the five-year survival rate for prostate cancer in the United States is 99 percent. In fact, most men diagnosed with prostate cancer will die of other causes without treatment. That is, what kills them while they have prostate cancer is generally not the cancer itself. The median age of diagnosis for prostate cancer is 66 and the median age of death is 80. As with any cancer, the progression of the cancer is important for determining the treatment and survival outlook. Due to our extensive testing programs, 80.7 percent of prostate cancer diagnoses are due to the location of a tumor still within the prostate, and the five-year survival rate for local stage prostate cancer is 100 percent.
Treatment Options
The most common treatment methods for prostate cancer are watchful waiting or active surveillance. This is largely due to the comparative harmlessness most people experience with early stage, slow growth prostate cancer.  However, surgery to remove the tumor can leave the patient incontinent, due to the prostate’s proximity to the bladder, or with no natural reproductive function, which makes many men hesitant to undergo surgery. Most cases will never need surgery, and instead will use other extremely effective courses of treatment.
However, surgery to remove the tumor can leave the patient incontinent, due to the prostate’s proximity to the bladder, or with no natural reproductive function, which makes many men hesitant to undergo surgery. Most cases will never need surgery, and instead will use other extremely effective courses of treatment.
Prostate cancer is the second most commonly diagnosed cancer in the United States, which has led to dramatic increases in treatment options and survival rates in the last 40 years. However, that doesn’t mean there isn’t cause for concern. If you are diagnosed with prostate cancer, work closely with your physicians to pursue the right treatment.
More
 It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes.
It’s scary to receive a diagnosis of pancreatic cancer. It’s even scarier when you’re not a candidate for surgery, the most effective treatment for pancreatic cancer that has not yet spread. Only about 20 percent of pancreatic cancer patients receive a diagnosis before the cancer spreads, and of those, some will not be healthy enough to undergo surgery due to conditions like heart disease, chronic obstructive pulmonary disease or diabetes. Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.
Physicians at Henry Ford Hospital in Detroit wanted to investigate the effectiveness of SBRT for treating pancreatic cancer in patients who are not good candidates for more aggressive traditional treatments, like surgery, chemotherapy, or traditional radiation therapy. In a study published in 2010, they offered SBRT treatments to 12 patients with inoperable stage I or stage II pancreatic cancer. Each patient received three to seven treatments. The average age of the patients was 83 years.